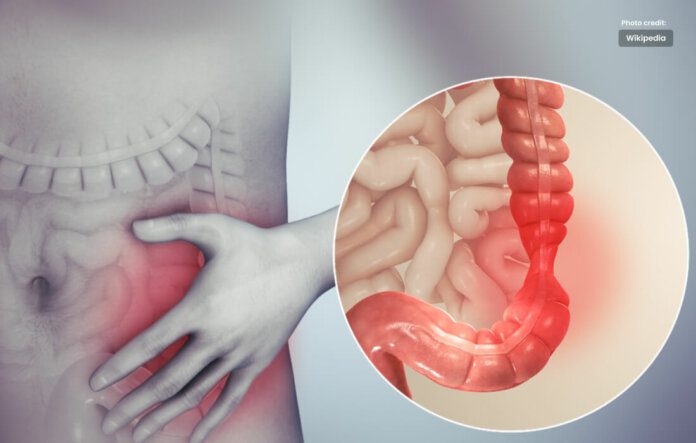
Abdominal pain, discomfort in IBS. Previously known by different names.
- IBS Colitis
- Mucous Colitis
- Spastic Colon
- Nervous Colon
- Spastic Bowel
The disorder comes in four different forms in IBS:
- IBS with constipation (IBS-C)
- IBS with diarrheas’ (IBS-D)
- Constipation and diarrheas’ alternate over the course of mixed IBS (IBS-M).
- For those who don’t fit into the aforementioned kinds, there is unsub typed IBS (IBS-U).
IBS is not a life-threatening condition, nor does it increase your risk of developing colon cancer, Crohn’s disease, or other gastrointestinal disorders. However, it could become a persistent issue that alters your way of living.
IBS sufferers may skip work or school more frequently and may feel less capable of engaging in regular activities.
Some people may need to adjust their work environment, whether it be by working from home, working less hours, or perhaps taking time off altogether.
Symptoms of IBS
People who have IBS may have the following symptoms:
- Diarrhea (often characterized as violent diarrheal bouts)
- Constipation
- Diarrhea alternating with constipation
- Cramps or sensations in the lower part of the stomach, which are typically stronger after eating and subside after a bowel movement
- Excessive gas or bloating
- Stools that are harder or looser than usual (pellets or flat ribbon stools)
- Belly that protrudes
- Your faces contains mucus
- Feeling the desire to poop even if you just did
- Food sensitivity
- Tiredness
- Anxiety
- Depression
- Acid reflux and indigestion
- Headaches
- Constant need to pee
These symptoms can occasionally be caused by other reasons. If you have IBS, you probably have these symptoms every week for three months or less frequently for at least six months.
IBS symptoms in women may worsen around the time of their period. Some patients also experience sexual or urinary symptoms. Stress might exacerbate symptoms.
When to contact a doctor
Consult a physician if you experience an IBS symptom for a prolonged period of time, develop a new symptom, or experience pain that is worse than normal or that is new.
You should also visit a doctor if you typically take over-the-counter treatments but they are no longer relieving symptoms like diarrhea, gas, or cramps.
Inform your doctor if a condition concerns you despite your belief that it is not physically related to IBS.
Let your doctor know, for instance, if the issue is causing you tension, anxiety, or sleeplessness.
There are “red flags” to watch out for that could indicate something more serious is happening even if IBS often doesn’t lead to more serious disorders.
A symptom that is unusual for IBS is a red sign. See your doctor if you have one or more of them. To figure out what’s going on, testing will be required.
Red-flag signs consist of:
Rectal bleeding:
It can simply be a side effect of your constipation from irritable bowel syndrome, brought on by a tear in your anus.
Hemorrhoid may also be the source of the bleeding. However, you should seek medical assistance right immediately if you have a lot of blood in your stool or if the bleeding simply won’t stop.
Vomiting, Fever and Anemia:
Call your doctor if you believe you have one or more of them.
Weight loss:
It’s time to get it looked out if you notice that you’re losing weight without any apparent cause.
Causes and Risk Factors for IBS
Despite the fact that a number of things can produce IBS symptoms, nobody really knows what causes it.
According to studies, the colon becomes hypersensitive and overreacts to small stimuli. The gut muscles spasm instead of moving slowly and rhythmically. That can result in constipation or diarrhea.
However, to another notion, it can be related to body-produced substances like serotonin and gastrin that regulate nerve signals between the brain and digestive system.
Other researchers are examining whether specific intestinal bacteria can cause the illness.
Between 25 million and 45 million Americans suffer from IBS. People seem to be more prone to have it for the following reasons than for others:
Being a women
The illness affects around twice as many women as men. It’s unclear why, however some studies speculate that the fluctuating hormone levels during the menstrual cycle may be a factor. Studies to date have not supported this.
Age
IBS can afflict anyone at any age, however it seems to affect people most frequently between the ages of 40 and 50.
Medications
Studies have linked sorbitol-containing medications, antidepressants, and antibiotics to IBS symptoms.
Food sensitivities
Some people may have stomach distress after consuming dairy, wheat, fructose, a sugar found in fruits, or the sugar substitute sorbitol.
Alcohol, fizzy beverages, and fatty foods can all interfere with digestion. Although there is no evidence that any of these foods cause IBS, they might exacerbate symptoms.
Emotional trouble
Some IBS sufferers appear to have stress management issues, to have a mental illness, or to have had a traumatic incident like sexual assault or domestic violence. It’s unclear if stress or IBS manifests itself initially.
However, there is evidence that behavioral therapy and stress management can help some people with the illness manage their symptoms.
Family history
It appears that the illness runs in families. According to certain studies, your genes might be involved.
Other
Digestive issues, such as food poisoning, the stomach flu, or traveler’s diarrhea. According to a tiny study that was released in January 2021, the immune system may be altered by a GI tract illness, causing it to react to some foods as if they were pathogens or viruses. Researchers are studying these preliminary results.
IBS Diagnosis
The diagnosis of IBS cannot be made by particular laboratory tests. Your doctor will examine you to determine whether you have IBS and may order tests to rule out other disorders like:
- Poor eating habits and food allergies, such as lactose intolerance,
- Medications including antacids, iron, and certain high blood pressure medications
- Infection
- Deficiencies in the amount of enzymes the pancreas secretes to adequately digest or break down food
- inflammatory bowel conditions such as Crohn’s disease or ulcerative colitis
To determine if you have IBS, your doctor may do some of the following tests:
- Colonoscopy or a flexible sigmoidoscopy to check for indications of obstruction or inflammation in your intestines
- If you have indigestion or heartburn, get an upper endoscopy
- X-rays
- Blood tests to check for symptoms of infection, thyroid issues, and anemia (lack of red blood cells)
- Stool examinations for diseases or blood
- Tests for celiac disease, gluten sensitivity, and lactose intolerance
- Examinations to check for bowel muscle issues
IBS Care and Treatment
Though almost all IBS sufferers are eligible for assistance, no one treatment is effective for everyone. To manage your symptoms, the best treatment strategy will require collaboration between you and your doctor.
IBS symptoms can be brought on by a variety of factors, such as certain meals, medications, the presence of gas or stools, and emotional stress. You’ll have to identify your triggers. You might need to take medicine and adjust your lifestyle.
Changes in diet and lifestyle
IBS usually gets better over time with a few simple dietary and activity modifications. Here are some suggestions for reducing symptoms:
- Avoid the caffeine found in soda, tea, and coffee.
- Consume foods like fruits, vegetables, whole grains, and nuts to add fiber to your diet.
- Drink three to four glasses of water a day, at the very least.
- Avoid smoking.
- Learn to unwind by increasing your physical activity or lowering your stress levels.
- Limit your consumption of milk and cheese.
- Eat more frequent, smaller meals rather than larger ones.
- Keep a diet journal so you can identify the foods that trigger IBS attacks.
Red peppers, green onions, red wine, wheat, and cow’s milk are typical food “triggers”. Suppose you’re worried about obtaining enough calcium. In that case, you can try to get it from other foods like sardines, salmon with bones, tofu, yoghurt, broccoli, spinach, turnip greens, orange juice and bread that has calcium added to it, or calcium pills.
Your doctor might advise you to attempt a low-FODMAP diet, which limits the consumption of difficult-to-digest carbohydrates including wheat, beans, and specific fruits and vegetables.