Renal stenosis-related systemic hypertension angioplasty and stent.
To treat a narrowed renal artery, an angioplasty and stent are performed.
A tiny plastic tube is inserted into the compressed artery with the help of X-rays as a guide.
The narrowed portion of the artery is opened by blowing up a special balloon on the tube.
To maintain the artery open, a stent, an inflatable tube, is then inserted.
Abstract:
Though infrequently performed, percutaneous transluminal angioplasty and stent implantation is a well-known treatment for renovascular hypertension.
We describe a case of extreme renovascular hypertension caused by atherosclerotic renal arteries that was actually resolved by radial artery access strategy stent implantation.
Introduction:
Throughout this test case, we describe a young woman who developed severe secondary hypertension caused by renal artery atherosclerosis and was successfully treated with percutaneous transluminal angioplasty.
This case emphasizes a number of topics that are important to doctors, including the utilization of the Transradial method for successful renal artery intervention and the role of renal artery atherosclerosis as a secondary cause of malignant hypertension.
Case Presentation Of Angioplasty:
A 44-year-old woman with previously acceptable cholesterol (LDL 111 mg/dl), historically normal blood pressure (100/60 on average), no family history of early cardiovascular disease.
A BMI of 27, and no personal prior cardiovascular history, started experiencing headaches that were linked to blood pressure readings above 180 systolic.
For severe “essential hypertension,” she was put on a beta blocker and an ace-inhibitor and directed to a cardiologist.
Her blood pressure grew more challenging to manage over a three-month period despite efforts to do so with numerous medications (beta blockers, ace-inhibitors, thiazide diuretics, and ultimately aldosterone antagonists).
Secondary reasons were taken into consideration given her young age and the fast course of her hypertension.
kidney artery The right kidney was smaller (9.4 cm in length) than the left kidney (11.7 cm), with a higher peak systolic velocity of 306 cm/s.
Thus, turbulent flow distally in the artery (Figure 1A), both of which showed severe right renal artery stenosis.
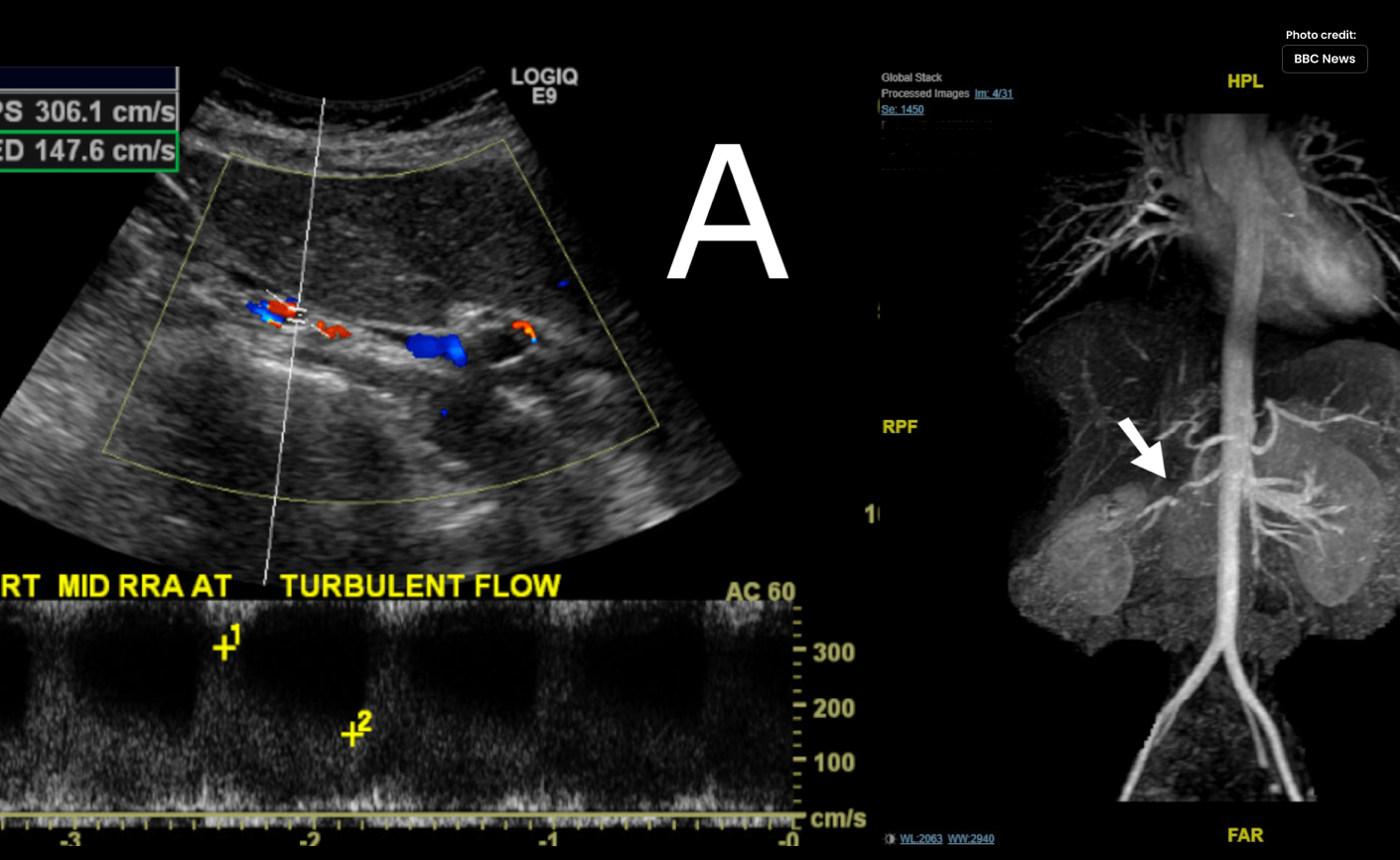
Renal artery in Figure 1. Magnetic resonance angiography and Doppler:
- “Right renal artery (Panel A) Doppler interrogation reveals higher velocities and turbulent flow, suggesting a hemodynamically considerable stenosis.”
- The right renal artery has a significant, selective stenosis, as shown by magnetic resonance angiography of the aorta and renal vasculature (Panel B).”
She was prepared for invasive angiography after magnetic resonance imaging (Figure 1B) revealed a significant, localized stenosis in the right renal artery.
A right radial access technique and a 5Fr Judkins catheter were used to perform a diagnostic renal angiography.
It verified that the left renal artery was normal and that the right renal artery had a considerable stenosis (Figure 2A).
The stenosis’ angiographic appearance was consistent with atherosclerosis since there was a clear reduction in blood flow to some areas of the proximal capillaries.
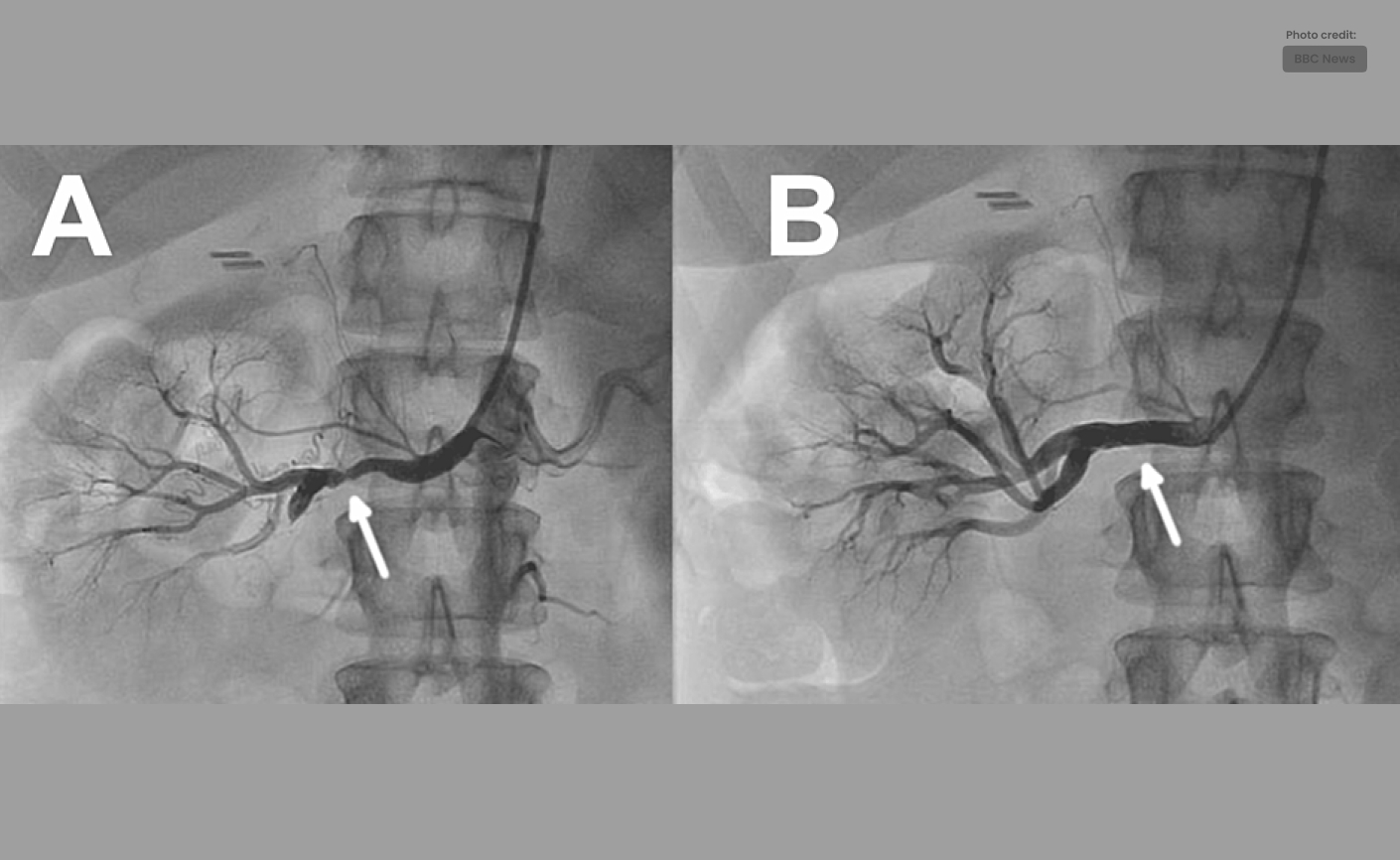
Figure 2: Renal artery angiography with stent implantation and pre- and post-angioplasty:
- “Angiogram of the right renal artery utilizing a multifunctional guide shows a high-grade atherosclerotic plaque in the middle of the artery (panel A).”
- “After stent insertion, the inferior branch of the renal artery is flowing normally and there is no stenosis left (panel B).”
Using a 100 cm multifunctional guide, percutaneous transluminal angioplasty and stent insertion were carried out.
A 2.5 x 12 mm balloon was used to inflate the lesion, and a drug-eluting Synergy Megatron stent from Boston Scientific, Marlborough, Massachusetts, was subsequently used to stent it (Figure 2B).
Instead of expressly choosing the type of stent based on any (theoretical) considerations of its drug-eluting properties, the size and availability of the device were taken into account.
The patient’s blood pressure was 121/80 three hours after the treatment before being discharge, contrasting to 179/113 the week before during an ER visit.
She stopped using all anti-hypertensive drugs after two weeks.
She is still normotensive and off of all meds more than a year later.
Discussion:
The vast majority of cases of renovascular hypertension (5% of all occurrences of hypertension) are caused by fibromuscular dysplasia and atherosclerotic renal artery disease.
There is evidence that percutaneous transluminal renal angioplasty and stenting in both of those categories can lower blood pressure, lessen acute pulmonary edoema, and stop the progression of renal failure [1].
It is acknowledged as a suitable therapy for unilateral (or bilateral) renal artery stenosis in the presence of accelerated/resistant hypertension.
However there are currently few randomized controlled trials to support this [2].
Although less frequently utilized, Transradial access is a recognized method for renal artery procedures.
Similar to coronary procedures, it has the potential to decrease post-procedure bed rest, access site problems, and patient dissatisfaction while still allowing successful intervention.
A cranio-caudal approach may be beneficial because to the angulation of the renal arteries in that coming from above the arteries may facilitate cannulation and support the delivery of equipment [4].
It’s important to be aware of several potential drawbacks or implications, such as the necessity for longer equipment for radial access and the possibility of trouble accessing the renal arteries in taller individuals.
In some cases, it might be essential to remove intervening equipment (backflow valves) or use the left-radial route [5].
Conclusions:
We offer this case as an illustration of secondary renovascular hypertension that was successfully managed by mechanically correcting a severe renal artery atherosclerotic stenosis.
Transradial access for percutaneous renal artery therapies may attract more attention as renal artery denervation becomes more likely to be used as a treatment for hypertension.
This instance also emphasizes how crucial it is to pursue a diagnosis based on clinical findings in patients who do not have major risk factors.
This is because doing so can lead to meaningful and advantageous treatment outcomes.